Zusammenfassung
Ultraschall neu interpretiert
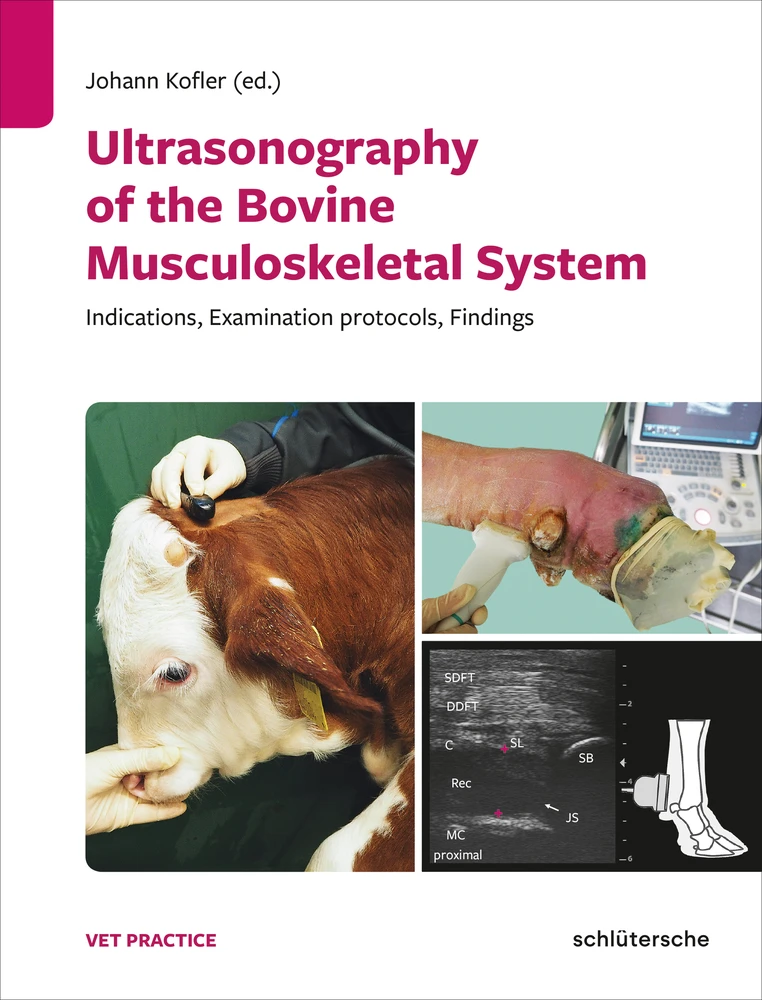
Die Ultraschalluntersuchung am Bewegungsapparat des Rindes ist an veterinärmedizinischen Kliniken weltweit als Routine-Untersuchung etabliert. Insbesondere in der Milchviehhaltung führen Lahmheiten bei Kühen schnell zu finanziellen Verlusten. Praktisch tätige Tierärzte können ihre vorhandenen Ultraschallgeräte problemlos nicht nur für gynäkologische, sondern auch für orthopädische Untersuchungen adulter Rinder und Kälber nutzen.
Dieses Praxisbuch gibt konkrete Anleitungen für die korrekte sonografische Untersuchung einzelner Gelenke. Als Orientierungshilfe für die Erstuntersuchung dient eine Beschreibung der jeweiligen anatomischen Leitstrukturen jeder Region. International tätige Spezialisten stellen in über 300 Abbildungen sonoanatomische Normalbefunde und sonopathologische Befunde häufiger Erkrankungen gegenüber. Ein Muss für moderne Rinderpraktiker, die ihren diagnostischen Horizont erweitern möchten!
Leseprobe
Inhaltsverzeichnis
- Cover
- Half Titelseite
- Titelseite
- Copyright
- Table of contents
- Authors
- Preface
- 1 Principles of ultrasonographic imaging of the bovine musculoskeletal system
- 1.1 Introduction
- 1.2 Physics and acoustic principles
- 1.2.1 Specular reflection
- 1.2.2 Diffuse reflection (scattering)
- 1.2.3 Attenuation
- 1.2.4 Axial, lateral and elevational resolution
- 1.3 Artifacts
- 1.3.1 Artifacts associated with resolution problems
- 1.3.2 Refraction or double image artifacts
- 1.3.3 Reverberation artifact
- 1.3.4 Comet-tail and ring-down artifacts
- 1.3.5 Distal acoustic enhancement
- 1.3.6 Distal acoustic shadowing artifact
- 1.3.7 Edge shadowing artifact
- 1.3.8 Fan or other electrical induced artifacts
- 1.4 Probes and frequencies
- 1.5 Preparation of the patient and the region of interest
- 1.6 Orientation and use of a standardized ultrasonographic examination protocol
- 1.7 Description of findings and documentation
- 2 Ultrasonography of arthritis, tenosynovitis, bursitis, abscesses, hematomas – general findings
- 2.1 Introduction
- 2.2 Ultrasonographic examination technique for exudate-filled cavities
- 2.3 Normal ultrasonographic appearance of joints, tendon sheaths and bursae
- 2.4 General ultrasonographic findings in arthritis, tenosynovitis, bursitis, abscesses and hematomas
- 2.4.1 Arthritis, tenosynovitis and bursitis
- 2.4.2 Abscesses and hematomas
- 2.5 Conclusions
- 3 Ultrasonographic examination of the distal and proximal interphalangeal joint regions
- 3.1 Introduction
- 3.2 Indications for ultrasonographic examination
- 3.3 Anatomy
- 3.4 Ultrasonographic examination procedure and anatomical landmarks
- 3.5 Normal ultrasonographic appearance of the anatomical structures
- 3.6 Sonopathological findings
- 3.6.1 Arthritis of the DIJ
- 3.6.2 Arthritis of the PIJ
- 3.6.3 Osteitis and osteomyelitis
- 4 Ultrasonographic examination of the metacarpo- and metatarsophalangeal joint regions
- 4.1 Introduction
- 4.2 Indications for ultrasonographic examination
- 4.3 Anatomy
- 4.4 Ultrasonographic examination procedure and anatomical landmarks
- 4.5 Normal ultrasonographic appearance of the anatomical structures
- 4.6 Sonopathological findings
- 4.6.1 Arthritis
- 4.6.2 Osteitis and osteomyelitis
- 4.6.3 Edema, abscesses and thromboses
- 4.6.4 Collateral ligament tears, luxation/ subluxation and adjoining physeal fracture
- 5 Ultrasonographic examination of the carpal region
- 5.1 Introduction
- 5.2 Indications for ultrasonographic examination
- 5.3 Anatomy
- 5.4 Ultrasonographic examination procedure and anatomical landmarks
- 5.5 Normal ultrasonographic appearance of the anatomical structures
- 5.6 Sonopathological findings
- 5.6.1 Carpal arthritis
- 5.6.2 Osteitis and osteomyelitis
- 5.6.3 Precarpal bursitis (precarpal hygroma)
- 5.6.4 Tenosynovitis of the carpal extensor and flexor tendon sheaths
- 5.6.5 Edema and abscesses
- 6 Ultrasonographic examination of the elbow region
- 6.1 Introduction
- 6.2 Indications for ultrasonographic examination
- 6.3 Anatomy
- 6.4 Ultrasonographic examination procedure and anatomical landmarks
- 6.5 Normal ultrasonographic appearance of the anatomical structures
- 6.6 Sonopathological findings
- 6.6.1 Arthritis
- 6.6.2 Osteitis and osteomyelitis
- 6.6.3 Fractures, subluxations and osteoarthrosis
- 7 Ultrasonographic examination of the shoulder region
- 7.1 Introduction
- 7.2 Indications for ultrasonographic examination
- 7.3 Anatomy
- 7.4 Ultrasonographic examination procedure and anatomical landmarks
- 7.5 Normal ultrasonographic appearance of the anatomical structures
- 7.5.1 Scapula and humerus
- 7.5.2 Scapulohumeral joint, bicipital and infraspinous bursa
- 7.5.3 Tendons and muscles
- 7.6 Sonopathological findings
- 7.6.1 Arthritis
- 7.6.2 Bursitis
- 7.6.3 Osteomyelitis, osteitis, avulsion fractures and luxation
- 7.6.4 Periarticular abscess
- 8 Ultrasonographic examination of the tarsal region
- 8.1 Introduction
- 8.2 Indications for ultrasonographic examination
- 8.3 Anatomy
- 8.4 Ultrasonographic examination procedure and anatomical landmarks
- 8.5 Normal ultrasonographic appearance of anatomical structures
- 8.6 Sonopathological findings
- 8.6.1 Tarsal arthritis
- 8.6.2 Lateral tarsal hygroma/bursitis
- 8.6.3 Disorders of the calcaneal tuber region
- 9 Ultrasonographic examination of the stifle region
- 9.1 Introduction
- 9.2 Indications for ultrasonographic examination
- 9.3 Anatomy
- 9.4 Ultrasonographic examination procedure and anatomical landmarks
- 9.5 Normal ultrasonographic appearance of the anatomical structures
- 9.6 Sonopathological findings
- 9.6.1 Stifle arthritis
- 9.6.2 Osteitis, osteomyelitis and osteochondrosis
- 9.6.3 Stifle ligament and meniscal injuries
- 9.6.4 Stifle bursitis
- 9.6.5 Abscesses and seromas
- 10 Ultrasonographic examination of the coxofemoral joint and pelvic region
- 10.1 Introduction
- 10.2 Indications for ultrasonographic examination
- 10.3 Anatomy
- 10.4 Ultrasonographic examination procedure and anatomical landmarks
- 10.5 Normal ultrasonographic appearances of the anatomical structures
- 10.6 Sonopathological findings
- 10.6.1 Coxofemoral arthritis
- 10.6.2 Coxofemoral luxation
- 10.6.3 Fractures
- 10.6.4 Degenerative joint disease
- 10.6.5 Muscle lesions, abscesses, hematomas, nerve injuries, thromboses and tumors
- 11 Ultrasonographic examination of flexor and extensor tendons, tendon sheaths and the suspensory ligament
- 11.1 Introduction
- 11.2 Indication for ultrasonographic examination
- 11.3 Anatomy
- 11.4 Ultrasonographic examination procedure and anatomical landmarks
- 11.5 Normal ultrasonographic appearance of the anatomical structures
- 11.6 Sonopathological findings
- 11.6.1 Tear or rupture of tendons/ligaments
- 11.6.2 Septic inflammation of tendon sheaths and tendons
- 12 Ultrasonographic examination of muscles
- 12.1 Introduction
- 12.2 Indication for ultrasonographic examination
- 12.3 Anatomy
- 12.4 Ultrasonographic examination procedure and anatomical landmarks
- 12.5 Normal ultrasonographic appearance of the anatomical structures
- 12.6 Sonopathological findings
- 13 Ultrasonographic examination of limb vessels
- 13.1 Introduction
- 13.2 Indication for the ultrasonographic examination
- 13.3 Anatomy
- 13.4 Ultrasonographic examination procedure
- 13.5 Normal ultrasonographic appearance of arteries and veins
- 13.6 Sonopathological findings
- 13.6.1 Thrombosis
- 13.6.2 Calcinosis
- 13.6.3 Varicosity
- 13.6.4 Pathological PW-Color Doppler flow characteristics
- 14 Ultrasonographic imaging of bone lesions
- 14.1 Introduction
- 14.2 Indication for ultrasonographic examination of the bone
- 14.3 Anatomy of bone
- 14.4 Normal ultrasonographic appearance of bone surfaces
- 14.5 Ultrasonographic findings on bone surfaces
- 14.5.1 Fractures and fissures
- 14.5.2 Subluxation and luxation
- 14.5.3 Osteitis and osteomyelitis
- 14.5.4 Bone sequestrum
- 14.5.5 Osteochondrosis and osteoarthrosis
- 14.5.6 Bone-associated tumors
- 14.6 Conclusions
- 15 Ultrasonographic imaging and measurement of sole horn and digital fat cushion thicknesses
- 15.1 Introduction
- 15.2 Indication for ultrasonographic examination
- 15.3 Anatomy
- 15.4 Ultrasonographic examination procedure and anatomical landmarks
- 15.5 Normal ultrasonographic appearance of the anatomical structures
- 15.6 Sonopathological findings
- 15.6.1 Thin soles
- 15.6.2 Changes in the digital cushion (sole’s soft tissue) thickness
- 15.6.3 Alterations of the surface of the distal phalanx
- 15.6.4 Fractures of the pedal bone
- 16 Ultrasonographic measurement of backfat thickness
- 16.1 Introduction
- 16.2 Indications for ultrasonographic measurement of BFT
- 16.3 Anatomy
- 16.4 Ultrasonographic examination procedure and anatomical landmarks
- 16.5 Normal ultrasonographic appearance of the anatomical structures
- 16.6 Reference values for different breeds
- 16.7 Correlation of BFT with BCS
- 17 Ultrasonographic imaging of large nerves and ultrasound-guided nerve blocks of the limbs
- 17.1 Introduction
- 17.2 Principles of ultrasound-guided nerve block
- 17.2.1 Advantages of ultrasound guided nerve block
- 17.2.2 Needle insertion technique
- 17.3 Indications for ultrasound-guided nerve blocks
- 17.3.1 Indications for forelimb anesthesia: brachial plexus block
- 17.3.2 Indication for hindlimb anesthesia: sciatic and femoral nerve block
- 17.4 Anatomy of the brachial plexus and the sciatic and femoral nerves
- 17.4.1 Brachial plexus
- 17.4.2 Sciatic nerve
- 17.4.3 Femoral nerve
- 17.5 Ultrasonographic examination procedure and anatomical landmarks
- 17.5.1 Brachial plexus
- 17.5.2 Sciatic nerve
- 17.5.3 Femoral nerve
- 17.6 Normal ultrasonographic appearance
- 17.6.1 Normal ultrasonographic appearance of the brachial plexus
- 17.6.2 Normal ultrasonographic appearance of the sciatic nerve
- 17.6.3 Normal ultrasonographic appearance of the femoral nerve
- 17.7 Sonopathological findings
- 18 Ultrasonographic imaging of the spinal cord
- 18.1 Introduction
- 18.2 Indication for spinal ultrasonography
- 18.3 Anatomy
- 18.4 Ultrasonographic examination procedure for the spinal cord and anatomical landmarks
- 18.5 Normal ultrasonographic appearance of the spinal cord in the three acoustic windows
- 18.5.1 Atlanto-occipital acoustic window
- 18.5.2 Lumbar acoustic window
- 18.5.3 Lumbo-sacral acoustic window
- 18.6 Ultrasound-guided collection of cerebrospinal fluid
- 18.7 Sonopathological findings of the spinal cord
- 19 Ultrasound-guided joint and soft tissue interventions
- 19.1 Introduction
- 19.2 Indications for ultrasound-guided joint and soft tissue interventions
- 19.3 Application procedure
- Appendix
- References
- Index
Authors
Birgit Altenbrunner-Martinek Dr. med. vet.
Department of Farm Animals and Veterinary Public Health
University Clinic for Ruminants,
University of Veterinary Medicine Vienna
Veterinärplatz 1
1210 Vienna, Austria
 birgit.altenbrunner-martinek@vetmeduni.ac.at
birgit.altenbrunner-martinek@vetmeduni.ac.at
Kurt Bach DVM
Department of Veterinary Clinical Sciences
Faculty of Health and Medical Sciences,
University of Copenhagen
Højbakkegaard Allé 5
2630 Taastrup, Denmark
Javier Blanco Murcia Associate Prof., DVM
Department of Animal Medicine and Surgery
Faculty of Veterinary Medicine,
Complutense University of Madrid
Ciudad Universitaria
Avda. Puerta de Hierro, s/n.
28040 Madrid, Spain
Naida Cristina Borges Prof., DVM
School of Veterinary and Animal Science
Federal University of Goiás
Caixa Postal 131, Campus Samambaia
CEP: 74001-970 Goiânia, Goiás, Brasil
Sébastien Buczinski Prof., Dr. Vét., DÉS, MSc, DACVIM
Bovine Ambulatory Clinic
Faculty of Veterinary Medicine, University of Montréal
3200 Rue Sicotte
St-Hyacinthe, J2S 2M2, Qc, Canada
Sonja Franz Associate Prof, Dr. med. vet.
Department of Farm Animals and Veterinary Public Health
University Clinic for Ruminants,
University of Veterinary Medicine Vienna
Veterinärplatz 1
1210 Vienna, Austria
Arcangelo Gentile Prof., Dr. med. vet., Dip. ECBHM
Department of Veterinary Medical Sciences
University of Bologna
Via Tolara di Sopra 50
40064 Ozzano Emilia, Bologna, Italy
Maike Heppelmann PD, Dr. med. vet.
Clinic for Cattle
University of Veterinary Medicine Hannover, Foundation
Bischofsholer Damm 15
30173 Hanover, Germany
 maike.heppelmann@tiho-hannover.de
maike.heppelmann@tiho-hannover.de
Johann Kofler Associate Prof., Dr. med. vet., Dip. ECBHM
Department of Farm Animals and Veterinary Public Health
University Clinic for Ruminants,
University of Veterinary Medicine Vienna
Veterinärplatz 1
1210 Vienna, Austria
Isabelle Masseau Associate Prof., DMV, PhD, DACVR
Department of Sciences Cliniques
Faculté de Médecine Vétérinaire,
University of Montréal
3200 Rue Sicotte
St-Hyacinthe, J2S 2M2, Qc, Canada
Karl Nuss Prof., Dr. med. vet., DECVS, Dip. ECBHM
Department of Farm Animals
Vetsuisse-Faculty, University of Zurich
Winterthurerstrasse 260
8057 Zurich, Switzerland
Harald Pothmann Dr. med. vet.
Department of Farm Animals and Veterinary Public Health
Clinical Unit for Herd Health Management in Ruminants
University Clinic for Ruminants,
University of Veterinary Medicine Vienna
Veterinärplatz 1
1210 Vienna, Austria
 harald.pothmann@vetmeduni.ac.at
harald.pothmann@vetmeduni.ac.at
Michela Tatiana Re Associate Prof., Dr. med. vet.
Department of Animal Medicine and Surgery
Faculty of Veterinary Medicine,
Complutense University of Madrid
Ciudad Universitaria
Avda. Puerta de Hierro, s/n.
28040 Madrid, Spain
Alexander Starke Prof., Dr. med. vet., Dip. ECBHM
Clinic for Ruminants and Swine
Faculty of Veterinary Medicine, University Leipzig
An den Tierkliniken 11
04103 Leipzig, Germany
 alexander.starke@vetmed.uni-leipzig.de
alexander.starke@vetmed.uni-leipzig.de
Adrian Steiner Prof., Dr. med. vet., DECVS, Dip. ECBHM
Farm Animal Clinic
Vetsuisse-Faculty, University of Berne
Bremgartenstrasse 109a
PO Box 3350
3001 Bern, Switzerland
 adrian.steiner@vetsuisse.unibe.ch
adrian.steiner@vetsuisse.unibe.ch
Preface
Ultrasonographic examination of the bovine musculoskeletal system was described in the mid-nineties for the first time and has become today a routinely applied ancillary diagnostic imaging technique in many veterinary teaching hospitals worldwide.
The goal of this textbook is to demonstrate to all cattle veterinarians the large variety of indications for ultrasonographic examination in bovine patients with musculoskeletal disorders. In particular, we want to provide detailed guidance on how the region of interest can be scanned correctly, which type and frequency of probes are adequate, to present the normal ultrasonographic appearance and to illustrate the most common pathological conditions.
We are required to make decisions during each clinical/orthopedic examination. However, clinical/orthopedic findings alone are often not sufficient to reach a diagnosis in bovine orthopedic patients. The additional use of diagnostic ultrasound may enable the clinician to state a definitive diagnosis, and to make a well-founded decision regarding prognosis and treatment. This includes the targeted administration of antimicrobial agents.
“Ultrasonography is the continuation of the clinical examination with other tools”: This statement was made in 1976 by the medical internist G. Rettenmaier, and still today I believe it precisely describes the paramount value of diagnostic ultrasound for the clinician in daily practice. It can be applied independently of location and time. Similar to the clinical exam, which follows a given examination schedule, the accurate ultrasonographic examination adheres to a standardized protocol, where the sonographer scans all the structures located in the region of interest in a certain sequence, in order to not overlook lesions, masses, or incriminated structures, which may not be clinically apparent.
Furthermore, the ultrasound probe is employed by the sonographer much like the fingers of his/her own hand during a clinical exam: The sonographer uses the probe for so-called sonopalpation, to classify the content of synovial cavities or other swellings as liquid, semi-solid, or solid effusions, to differentiate limb arteries and veins, and to diagnose thrombus formation.
The advantage of uniting the clinician and sonographer is that this person is fully familiar with the anatomic site in question as well as the clinical findings. Diagnostic ultrasound is a safe and non-invasive procedure for the patient, the sonographer and nearby personnel. Moreover, it is well suited for serial examinations to monitor the progression of the condition and response to treatment.
This is the first textbook on bovine musculoskeletal ultrasound composed by international experts that covers all parts of the bovine musculoskeletal system that can be involved in patients presented with lameness. The chapters in this textbook focus on specific joint regions of the limbs (e.g. fetlock, carpal, tarsal and other joint regions). These correspond to common experience with bovine orthopedic patients, where mainly one limb region is affected, but also occasionally where there is more than one defined limb region involved (most frequently in calves).
Each chapter is structured in the same manner: After a brief introduction, important indications for the ultrasonographic examination of individual regions are listed, followed by a brief anatomical overview, the presentation of anatomical landmarks and standard ultrasonographic views for the region of interest. This is followed by a detailed description of the ultrasonographic examination method for the particular region, and the normal ultrasonographic appearance of the most important anatomical structures. Finally, the ultrasonographic findings of the most common pathological conditions of the particular region are presented. Many sonograms illustrating normal appearances and the ultrasonographic findings of the most frequent disorders complete each chapter.
Additionally, there is an introductory chapter explaining the most important principles of diagnostic ultrasound, and the most common artifacts encountered during ultrasonographic examination. This textbook also contains a chapter on ultrasonographic imaging and measurement of the thickness of sole horn and the sole’s soft tissue layer, which is an important research topic today. This is completed by a chapter on the ultrasonographic measurement of the back fat thickness.
Besides the description of the ultrasonographic inspection of all (joint) regions of the limbs, additional chapters focus on the general ultrasonographic evaluation of synovial cavities, tendons and ligaments, muscles, vessels, large peripheral nerves and the spinal cord. These structures are important for the physiological function of the bovine musculoskeletal system. Maybe surprising for ultrasound newcomers, one chapter focuses on the ultrasonographic examination of bone surfaces and imaging of numerous associated bone alterations. The textbook is completed by a chapter on ultrasound- guided centesis of synovial cavities, ultrasound-guided fine-needle aspiration and biopsy collection.
I want to sincerely thank all the internationally recognized experts and authors for their contributions to this textbook, enabling a unique and comprehensive overview of all the indications and possible applications of diagnostic ultrasound in bovine orthopedic patients.
The authors of this textbook would like to encourage all cattle veterinarians in clinics and, in particular, in bovine practice, to improve their ultrasonographic regional skills of the bovine musculoskeletal system. We want to inspire bovine practitioners to use their already available ultrasound units and probes already used for bovine reproduction to improve diagnosis of bovine musculoskeletal disorders.
My proposed slogan for enthusiastic colleagues all over the world engaged in cattle (and of course with other species) health management is: Diagnostic ultrasound is the best friend of the clinician, it is available everywhere and at any time, and it is well suited to support immediate decision making in clinics and on-farm settings.
When a thorough clinical/orthopedic examination does not lead to a final diagnosis, always ask your best friend. When you visit an orthopedic bovine patient, follow the slogan “yes, we scan”!
Vienna, February 2021
Johann Kofler
Acknowledgements
I wish to thank Cameron R. McCulloch, PhD, University of Veterinary Medicine Vienna, for reading the text and providing language assistance.
I would like to acknowledge Mrs. Anna E. Vogl (Mödling, Austria); she designed all the illustrations that are attached to all sonograms demonstrating the exact placement of the probe to achieve the presented ultrasonographic image.
1 Principles of ultrasonographic imaging of the bovine musculoskeletal system
Sébastien Buczinski, Isabelle Masseau
1.1 Introduction
Ultrasonography is an imaging technique based on the reflection and refraction of acoustic waves as they are transmitted through the tissues (Kirberger 1995). In veterinary medicine, it was initially applied to the diagnosis of pregnancy, to assess reproductive organs prior to insemination or in an attempt to determine causes of failure to induce pregnancy in cattle. Its affordable cost and ease of use have contributed to its popularity and explain that today many veterinary practitioners are equipped with an ultrasound machine dedicated to cattle reproduction management programs (King 2006, DesCôteaux et al. 2009, Fricke et al. 2016).
In parallel with the development and sophistication of ultrasonographic examinations in the field of reproduction, a number of clinical conditions have emerged for which ultrasonography has been evaluated for its potential aid as a complementary imaging diagnostic tool. Over time, numerous research studies and growing expertise have resulted in diversification of ultrasound use in cattle leading to the recognition of its diagnostic utility for various indications, including examinations of musculoskeletal structures in cases of lameness, joint instability or penetrating wounds, among others (Flückiger 1997, Buczinski 2009a, Kofler 2009, Braun and Attiger 2016, Re et al. 2016b).
Ultrasonographic evaluation of musculoskeletal structures is facilitated by the superficial location of a majority of them. Consequently, most rectal probes (transducers) employed today for ultrasonography of the reproductive system can also be utilized for the evaluation of musculoskeletal structures. Since most practitioners are already equipped with ultrasound units, they do not have to pay additional costs for acquisition of new probes. Another important advantage of ultrasonography is its portability, allowing for musculoskeletal examinations to be performed directly on the farm (Ollivett and Buczinski 2016).
Like any other diagnostic imaging tool, it is important to understand the physical principles responsible for generating ultrasound images and commonly encountered artifacts (Kirberger 1995, Blond and Buczinski 2009). Understanding how artifacts occur can help their avoidance whenever possible or to use them advantageously to document the nature of the tissues from which they originate (e. g. gas in an abscess, osteophytes, dystrophic mineralization within a tendon, etc.). A few parameter settings that optimize image quality will also be briefly discussed. Therefore, the aim of this introductory chapter is to provide the reader with a brief overview of these important topics.
1.2 Physics and acoustic principles
Ultrasound consists of high frequency vibrations generated by the crystals within a probe. When subjected to an electric field, the crystals inside the probe become excited, which triggers a movement or vibration, generating the emission of the ultrasound wave. This phenomenon is based on the inverse piezo-electric effect of certain materials. The speed at which transmitted ultrasound waves are propagated through a structure of interest varies according to the type of medium.
The speed of ultrasound waves through soft tissues is generally constant at approximately 1,540 m/s (Blond and Buczinski 2009).
A wave can be transmitted through a medium, as well as reflected, refracted and attenuated. Other types of effects such as diffraction, polarization, dispersion and interference can also occur.
The interference effect mentioned above is of particular interest for ultrasound examinations that are performed in the proximity of other wave-generating materials or electronic devices, such as ventilation fans in a barn (Kirberger 1995, Blond and Buczinski 2009, Hindi et al. 2013).
Details
- Seiten
- ISBN (ePUB)
- 9783842691520
- Sprache
- Englisch
- Erscheinungsdatum
- 2022 (Januar)
- Schlagworte
- Ultraschall Sonografie Anatomie Lahmheiten Bewegungsapparat Ergüsse Entzündungen Frakturen Gelenke Klauen Muskuloskelettales System Muskeln Orthopädie Rind Sehnen abscess anatomy arthritis bovine claw fracture joint lameness muscle musculoskeletal system nerve orthopedic sonogram spinal cord tendon ultrasonography ultrasound